Aerobic exercise is a continuous activity using all the major muscle groups. It allows your heart rate to gradually increase to a target rate and keeps it at this level for some time. The term aerobic means "with oxygen," which means that the amount of oxygen that can make it to the muscles to help them burn fuel and move is the limiting factor for this type of activity.
Examples of aerobic exercise include:
- power walking
- cycling
- swimming
- aerobic session at the gym with cardio equipment (treadmill, stationary bike, elliptical)
Benefits of Aerobic Exercise
Research shows that the more active you are, the longer you can live. Regular exercise can improve your level of cardiovascular fitness even if you are living with heart disease.
Regular aerobic exercise can:
- improve your cardiovascular fitness. This means making your heart and lungs stronger and more efficient.
- make changes in your body composition such as:
- decreasing your waist size
- decreasing your body fat
- increasing your muscle mass
- improve your blood glucose (sugar) levels
- reduce your risk for developing additional diseases like type 2 diabetes, high cholesterol, hypertension, and certain types of cancer.
Aerobic Activity and Congenital Heart Disease
Physical activity and exercise are good and beneficial for health regardless of the underlying heart condition. Research has shown consistently that being “active” helps live better and longer.
Although in the past the general recommendations were to restrict physical activity for adults with congenital heart disease because of safety concerns, in recent decades more evidence showed how being active is not only safe, but it also improves their life expectancy and quality of life.
Aerobic exercise can directly affect the body's ability to sustain exercise, what we call exercise capacity or tolerance. We usually measure exercise capacity/tolerance with a cardiopulmonary exercise test (CPET). During the test, subjects breathe through a special mask or mouthpiece allowing us to measure the breathing gasses (the amount of oxygen you inhale, and the amount of carbon dioxide you exhale). One specific parameter called VO2 measured with this test reflects someone’s exercise capacity/tolerance. The greater the VO2, the higher the exercise capacity/tolerance.
VO2 and Health
The highest level of VO₂ an individual can achieve as measured during the CPET has been identified as the single best predictor of all-cause mortality (risk of dying).
If we think of the human body as a car, VO₂ represents the size of the car’s engine. The larger the engine, the higher the horsepower and higher the potential for performance is. During everyday activities, a larger engine will hardly ever be maxed out but if that engine gets too small completing simple tasks will cause the engine to reach its limit faster. As a result, even simple daily tasks, like walking from the couch to the kitchen, will become more challenging. VO2 naturally declines with age, meaning the older we get the lower our ability to sustain activities becomes. This declining trend of VO2 is faster in people living with a heart condition, however VO2 is trainable. With a proper prescription of exercise intensity and duration, VO2 can be increased, and this is the goal of the program.
In 2005 Dr. Diller and his colleagues published a study in Circulation (a renowned journal in cardiology) that looked at individuals with congenital heart disease and assessed the relationship between the level of VO2 and life expectancy and the need for hospitalizations. What they found was a real change of mindset. They demonstrated that the greater VO2, the greater life expectancy, and fewer hospitalizations (see figure below).
Aerobic activity in individuals with Fontan circulation. What do we know?
The Fontan circulation is a result of multiple surgeries that are now used to correct many different congenital heart defects. Learn more about Fontan Circulation (link to how my heart works - Fontan)
Until recently little was known about the effect of regular exercise on the Fontan circulation therefore the general recommendations regarding exercise were cautious and restrictive. Over the past decade, medical providers, as well as researchers, have been studying the effect of exercise on the Fontan circulation. The results of these studies have proven that through regular exercise and training, patients with Fontan physiology can increase their exercise capacity/tolerance, maintain a good cardiac function, and have a better quality of life. Based on this increasing amount of evidence, exercise has been integrated into the general recommendations for individuals with Fontan circulation.
Our recommendation is to regularly discuss the best way to safely exercise with your cardiologist and cardiac rehabilitation team.
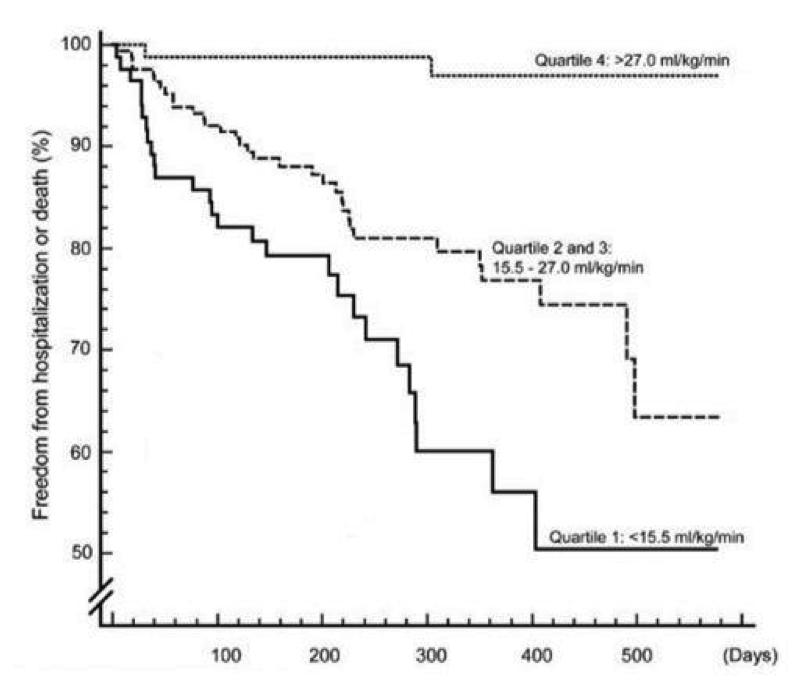
Fig 1. Survival curves for combined end-point of hospitalization or death (event-free survival). Patients were classified into increasing quartiles (1 through 4) of peak VO2 (the greater the better exercise capacity). Adapted from Diller GP et al. Exercise intolerance in adult congenital heart disease: comparative severity, correlates, and prognostic implication. Circulation. 2005 Aug 9;112(6):828-35
F.I.T.T. for Aerobic Exercise
Your cardiovascular prevention and rehab team prescribes your aerobic exercise in a similar way to how your doctor prescribes your medication.
Your doctor tells you to take a particular type of medication a certain number of times each day, at a certain dosage, and for a certain period. Your exercise prescription works the same way.
An easy way to remember how your program is prescribed is to use the FITT principle.
- Frequency, or how often you exercise.
- Intensity, or how hard you work
- Type, or what exercises you do.
- Time, or how long you exercise for.
The right dose of Exercise
Current guidelines on physical activity for adults 18 to 64 recommend 150 minutes of activity per week at moderate to vigorous intensity, which equals to at least 20 minutes of exercise per day. This is the minimum dose of exercise that will give someone who is regularly active the benefits of exercise.
Reducing your sedentary behavior with additional physical activity and trading light physical activity for more moderate to vigorous physical activity can provide greater health benefits.
Read more about the Canadian Guidelines
Intensity of Exercise
Determining how hard or at what level of intensity to exercise can be challenging.
The guidelines recommend exercising at a moderate to vigorous intensity, but what does this mean for you?
A cardiovascular prevention and rehabilitation team can develop an exercise prescription with the best and safest level of exercise for you.
Your exercise prescription will have some indicators to guide you reach the right intensity:
- a training heart rate range with a lower and higher limit
- a Borg Rating of Perceived Exertion (RPE)
Your exercise prescription is developed based on:
- your heart condition
- your current medical status
- medicines you take
- additional health concern you might have
- the results of a cardiopulmonary assessment
The cardiopulmonary exercise test (CPET) that you will undergo or already completed provides precise information about your exercise capacity/tolerance or V02 (maximal oxygen uptake), which is how well your body takes in oxygen and delivers it to your working muscle. Vo2 is the best indicator of your cardiopulmonary fitness level. The test also tells us how your heart rate and blood pressure respond to exercise.
Tips to make sure you are exercising at the right level
1. Check your heart rate
The heart rate increases during exercise because the heart needs to beat faster and harder to supply more oxygenated blood to your working muscles.
Measuring your heart rate during exercise will allow you to know if it is within the target range given by your cardiovascular prevention and rehabilitation team. What are the heart rate zones and why is it important for you to exercise within the range of heart rate zones provided by your cardiovascular prevention and rehabilitation team?
Heart rate zones are a percentage of your maximum heart rate (heartbeats per minute). Exercise too close to your maximum heart rate will make your heart and body struggle to keep up with the demands. The goal of heart rate zones is to make you exercise in the most efficient way but to allow you to challenge yourself to improve cardiovascular fitness or exercise tolerance.
If your heart rate is below your target range or if you feel you can increase the intensity of your exercise prescription, tell your cardiovascular prevention and rehabilitation team so that they can modify your exercise prescription.
Take your pulse
There are 2 areas where you can find your heart rate:
- Wrist, below the base of the thumb (radial artery)
Place 2 to 3 fingers on your wrist below the base of your thumb.
Press lightly until you feel your heartbeat.
- Neck below the angle of the jaw (carotid artery)
Place 2-3 fingers on the side of your neck (beside the groove under your jaw) in the hollow area. Press lightly until you feel your heartbeat.
Wearable devices can help you in monitoring your heart rate during your exercise. Commercial wearable devices measure heart rate and, some also measure heart rhythm. They are useful tool to monitor your heart rate during exercise if you were provided with heart rate target zones. They can also be used to track your daily steps and overall activity time. Several brands have different cost and accuracy of measures. If you feel that this device can help you starting an exercise routine you can discuss proper use with your cardiologist or rehabilitation team.
2. Use the rating of perceived exertion scale (RPE scale)
The Borg Rating of Perceived Exertion (RPE) scale will help you know how hard you’re working. It is used in monitoring the progress and intensity of exercise in individuals undergoing rehabilitation and endurance training.
Versions And Scoring
Borg's original version is a scale of 6-20; it has a high correlation to heart rate and multiplying each number by 10 gives the training heart rate as at the time of scoring.
To find your rating on the scale, think about your overall feelings of physical stress, effort, and fatigue.
- Don’t focus too much on any single thing, like leg tiredness or shortness of breath.
- Try to concentrate on your total, inner feeling of exertion.
See the scale below:
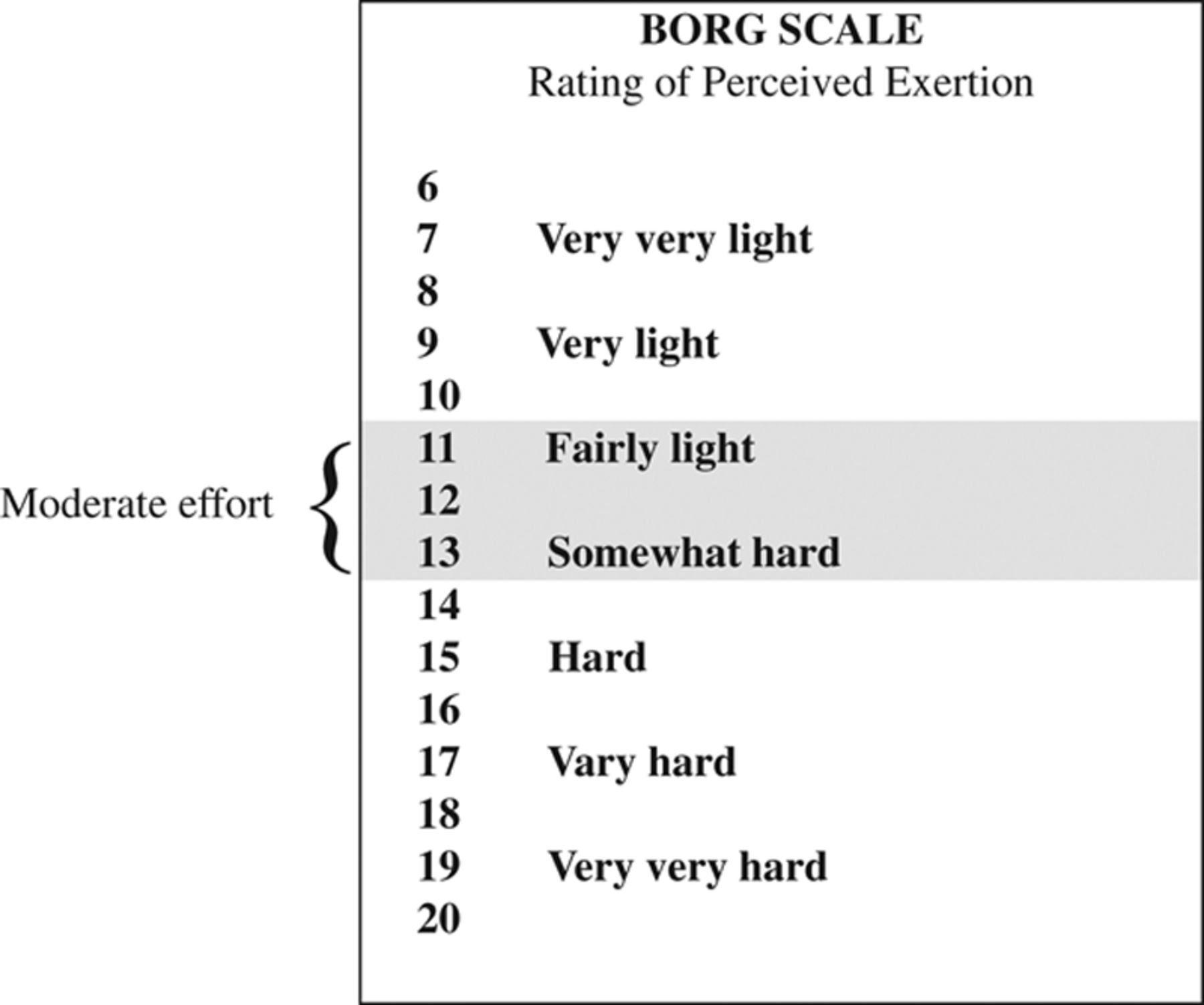
The scale was later modified to the Borg Dyspnoea Scale, which is mostly used in a specific area of the body for grading exertion sensations such as muscle pain or breathlessness.
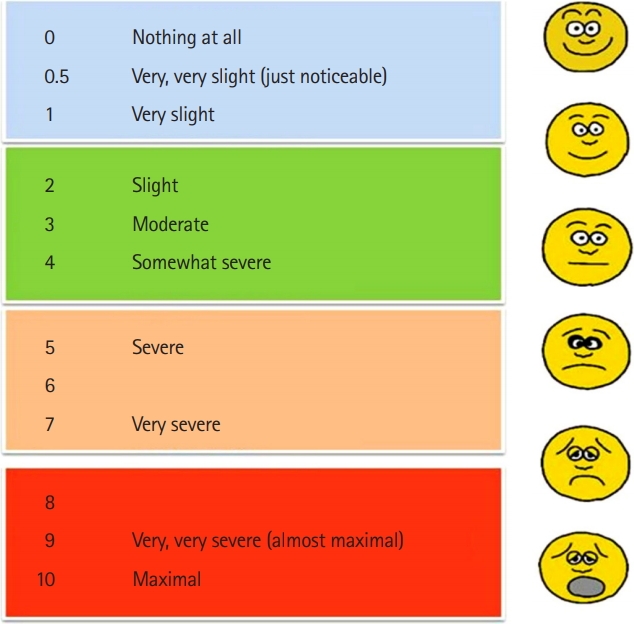
Find the best description of your level of effort from the examples on the right side of the table, and then find the number rating that matches that description.
- Ideally, your RPE will be between 4 and 6 during the exercise program.
- If your RPE is above these then the intensity is too high and will need to be adjusted.
3. Do the talk test
The Talk Test was developed to be an informal, subjective method of estimating appropriate cardiorespiratory exercise intensity. The method entails maintaining an intensity of exercise at which conversation is comfortable. When an individual reaches an intensity at which he or she can “just barely respond in conversation,” the intensity is safe and appropriate for cardiorespiratory endurance improvement.
In other words, you should be able to exercise and carry on a conversation without being overly short of breath. If you are exercising at moderate to vigorous intensity, you are still able to answer questions with a short phrase or yes and no answer but you won’t be able to carry on a conversation or sing a song. It is okay to hear yourself breathe while exercising.
4. Aim to have no symptoms while exercising
The “no pain, no gain” philosophy will take you outside a safe and optimal exercise intensity level.
If you experience any symptoms during your activities, it is important to lower the intensity of your exercise and speak with your cardiovascular prevention and rehabilitation team so that your prescription can be adjusted.
Symptoms you should take note of include:
- chest pain
- excessive shortness of breath
- dizziness
- light-headedness
- soreness
- muscle soreness joint
5. Your personalized exercise prescription
Your exercise prescription is designed specifically for you and is set at a safe and optimal level.
If you have questions or concerns regarding the intensity of the exercise, discuss it with your cardiovascular prevention and rehabilitation team and they will be able to explain how your program was developed.
Time/Duration of Exercise
For aerobic exercise, the duration of the activity could start at 10 minutes and progress up to 60 minutes. The duration of your exercise depends on your fitness level, medical history, and goals.
Type of Exercise
Aerobic exercise is a continuous whole-body rhythmic exercise that involves the large muscle groups of the body. This could include activities such as walking, cycling, jogging, dancing, and swimming. Aerobic exercise provides cardiovascular conditioning. The term aerobic means "with oxygen," which means that the amount of oxygen that can make it to the muscles to help them burn fuel and move is the limiting factor for this type of activity. Different factors are limiting the oxygen delivery to the muscle and therefore your exercise capacity:
- the heart function, main contributing factor
- the lung functions
- the ability of the blood to transport oxygen to the muscle
- the muscles ability to extract and utilize oxygen
Your exercise prescription is personalized, meaning it considers your heart condition, your pulmonary function, any blood and/or muscle condition that might affect your ability to exercise.
Warm-Up
Why is it Important to Warm-Up?
The purpose of a warm-up is to gradually prepare the heart, lungs, blood vessels, and muscles for safe and comfortable exercise.
Exercise increases the blood demand of the working muscles and the heart. A warm-up allows your blood vessels to open up and provides increased blood flow to the working muscles (such as the legs) and the heart muscle. This allows the body to exercise without too much physical stress at the beginning of any activity. This means:
- the demand and supply of oxygen to the heart muscle are in balance and increase gradually
- symptoms of chest pain, irregular heartbeats, dizziness, and shortness of breath are less common to happen during exercise.
How Do I Warm Up?
Your warm-up can be the same type of exercise you are going to do as part of your prescription but at a lower intensity for 5 to 10 minutes. For instance, if you exercise on a stationary bicycle, then cycle at a slow pedal speed, with little or no resistance.
Cool-Down
Why is it Important to Cool Down?
A cool-down reduces blood pooling (when blood collects in one area) in the legs. During exercise, blood flow to the muscles in your legs increases. If the extra blood in the legs is not returned to the upper body in a balanced way, blood will pool in the legs.
Your leg veins are next to the muscles in your leg. When you exercise, your leg muscles alternately contract and expand, pressing against the leg veins. The movements of the muscles help move the blood through the veins and back to the heart, the so-called “muscle pump”.
If you stop exercising suddenly, your leg muscles no longer help move blood back to the heart. This means that the amount of blood flowing into the legs is greater than the amount of blood flowing back to the heart, and the blood begins to pool in the legs.
With less blood returning to the heart than leaving it, there is less blood to fill the heart and less blood for the heart to pump out. The reduced blood flow to the heart and head could cause you to experience chest pain, skipped beats, or light-headedness.
During a cool-down, the leg muscles continue to move and to help pump blood back to the heart. This reduces blood pooling in the legs. Because blood flow to the heart and head has been maintained, you are less likely to experience problems.
How Do I Cool Down?
Your cool-down can be the same type of exercise you performed during your exercise session for 5 to 10 minutes at a lower intensity. For instance, if you exercise on a bicycle, cool down by cycling at a slow pedal speed with little resistance for at least 5 minutes.
Stretching
Stretching exercises are sometimes referred to as warm-up or cool-down exercises. Do not confuse stretching exercises with your cardiovascular warm-up and cool-down exercises.
Stretching your muscles (flexibility training) is an important part of your physical fitness. Stretching improves the flexibility of your muscles and reduces the risk of injury when doing aerobics and resistance training.
Static stretching involves holding a position for some time. It is important to do at least 5 minutes of cardiovascular warm-up before stretching a muscle. A good time to stretch is after your aerobic training when your muscles are already warm.
How Do I Stretch?
To do a static stretch, stretch to the farthest point you comfortably can. You should feel tightness, but the stretch should not cause pain or discomfort in the muscle. Hold the stretch while continuing to breathe for 15-30 seconds.
Remember not to bounce or change position while you are holding the stretch.
Exercise Indoors
There are several ways to stay active indoors, below are some examples:
- Community Centers and Gym facilities: Find a community center or a gym in your area.
- Mall Walking: Mall walking is a great free alternative for indoor walking.
- At Home: Exercise equipment (such as a treadmill, stationary bicycle or elliptical machine), is a great way to stay active in the comfort of your own.
- Exercise videos available online on YouTube are also another way you can stay active indoors.
When to Skip Exercise
Normally, it is best to exercise daily. But there are some times when you should skip (take time off) your exercise sessions.
Take time off your exercise plan if:
- You are sick. Avoid exercise if you have an infection like the flu or a cold. Your body needs rest during this time. If you exercise, your body has a harder time fighting the infection. When you are better, restart your exercise gradually (less time and slower). The amount of time you took off from your exercise should be the same amount of time it takes to get back to your regular exercise routine.
- You are injured, such as a pulled muscle. If you have a new injury that you are concerned about, talk to your family doctor. Your doctor and your cardiovascular prevention and the rehabilitation team will help you decide on the best way to get better and when it is safe to return to your exercise program.
- You have symptoms. You should not feel unwell during your exercise. Know what to do if you feel symptoms like chest pain or shortness of breath during your exercise »
- You have skipped your medication for your last 2 days. Check with your rehabilitation team when it is safe to restart your exercise program or routine.
